Australia’s Cervical Cancer Screening: Safer, Smarter and Simpler
Australia continues to lead in cervical cancer prevention, with one of the lowest rates of cervical cancer and related deaths in the world1. This success is largely due to the introduction of the National Cervical Screening Program (NCSP) in 1991 and the National Human Papilloma Virus (HPV) vaccination program in 2007.
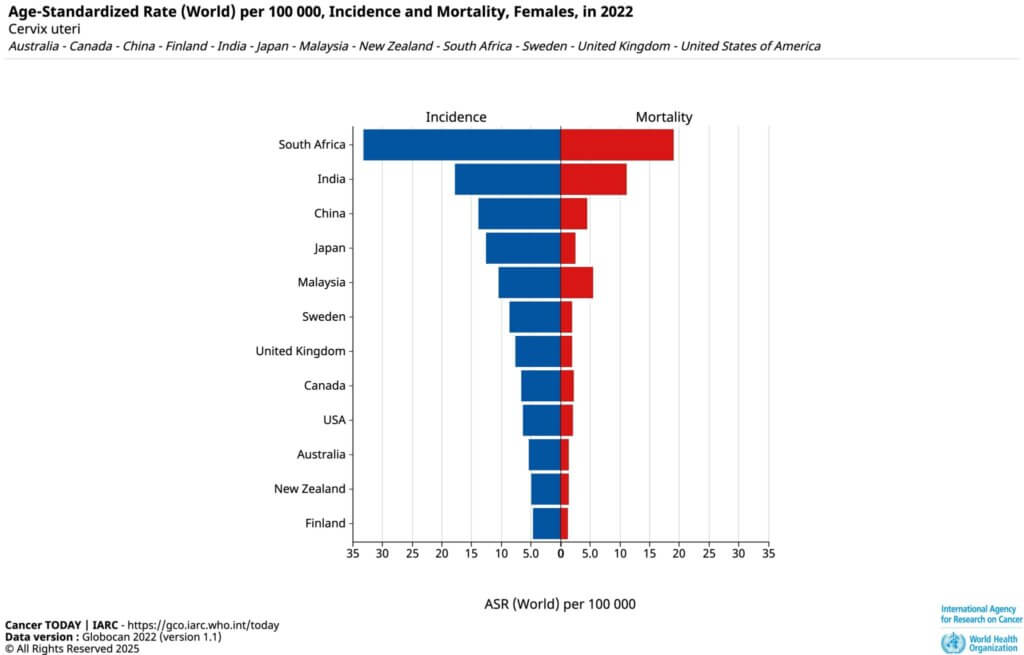
Global cervical cancer incidence and mortality rates in 2022: Bar chart comparing age-standardised rates per 100,000 women across 14 countries. Source: IARC Globocan 2022
As of 14 April 2025, important changes have been made to improve accuracy, accessibility and comfort for those undergoing cervical screening in Australia.
Quick facts about Cervical Cancer in Women
- It’s preventable with regular screening and HPV vaccination
- Commonly caused by HPV — a common virus most people encounter
- Early stages show no symptoms — making routine screening vital
- Cervical Screening Tests detect early changes before cancer develops
- HPV vaccine is most effective before exposure, but can still be beneficial later
- Early treatment is highly effective
Find out more from the Cancer Council.
Why Cervical Screening Is Now Every 5 Years (Not 2)?
Before 2017, people were routinely advised to have a Pap smear every two years. Today, that advise has changed – and for good reason.
Australia now uses a more advanced Cervical Screening Test that checks for human papillomavirus (HPV), the virus responsible for nearly all cervical cancers. The new test is different from the old Pap Smear test. The old test looked for abnormal cells after changes had started. The new test finds HPV before any problems develop.
HPV changes in the cervix take a long time to develop. Because of this, it is safe to get screened every five years if your test result is negative. This approach is also more effective.
Bonus: This evidence-based change is expected to reduce cervical cancer cases and deaths by at least 20%2..
🛑 Important note: Cervical screening is designed for people without symptoms. Fast-growing, aggressive cancers are extremely rare, and they are typically picked up when a person visits their doctor due to symptoms — such as pain, bleeding or something that just doesn’t feel right.
So if something feels off, don’t wait for your next screening — see your GP as soon as possible.
2025 Cervical Screening Updates: What’s Changed?
- Self-Collection Is Now Available to Everyone
Anyone eligible for cervical screening in Australia can now collect their own sample. They can use a simple vaginal swab at the GP clinic or at home. It’s just as accurate as a doctor-collected sample and can help more people feel comfortable with screening.
If you had an abnormal cervical screening result before, your doctor might let you self-collect. This choice will depend on your situation and the advice you receive.
- Simplified Follow-Up After Abnormal Results
If you’ve had treatment for high-grade changes (HSIL), follow-up (also known as the Test of Cure) now involves:
- One HPV test every 12 months for two years
- If both results are negative, return to the 5-year screening schedule
- Updated Screening for People Without a Cervix
If you had a total hysterectomy, which means your uterus and cervix were removed, your follow-up is easier. This is especially true if you had high-grade changes. You will have an annual HPV test or combined testing (HPV + Pap smear). This continues until you get two negative results in a row.
- Improved Monitoring for Adenocarcinoma in Situ (AIS)
For those previously treated for AIS:
- Annual screening is recommended for 5 years post-treatment
- If all results are negative, testing every 3 years is recommended
- After 25 years of normal results, revert to 5-yearly screening
Cervical Screening in Australia: What You Need to Know
- Who should screen: Anyone aged 25 to 74 who has ever been sexually active.
- How often: Every five years if your result is negative.
- Screening options: Choose between a self-collected swab or a doctor-collected sample.
- Post-treatment: Follow-up care is now simpler and clearer.
Queensland Health has some good videos here if you have further questions about cervical screening.
Australia’s Goal: Eliminate Cervical Cancer in Women by 2035
With these updates, Australia aims to be the first country in the world to eliminate cervical cancer as a public health problem. By making screening more accessible and accurate, the NCSP is leading the way in cancer prevention.
Check your eligibility or book an appointment for your screening with one of our experienced GPs today.
References:
- Globocan. Section of Cancer Surveillance 2015. International Agency for Research on Cancer (IARC); 2012 [cited 2015 Oct 23].
- Cancer Council – Eliminating Cervical Cancer by 2035.
- Queensland Health. Videos about Cervical Screening – Cervical Screening made simple.