Heavy Periods and Painful Periods: What You Need to Know
by Dr Lu-Ann Chan
As a GP, one of the most common questions I get from women is that they suffer from heavy and/or painful periods. From the time a girl reaches puberty, dealing with periods becomes a regular part of life. But for some, it’s more than just a few days of inconvenience – it’s heavy bleeding that feels never-ending or excruciating pain that makes daily activities seem impossible. In this article, allow me break down why some women experience heavy periods, how common it is and what can be done about it.
Understanding Heavy Periods:
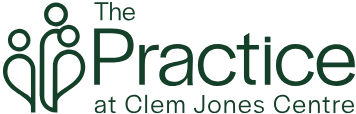
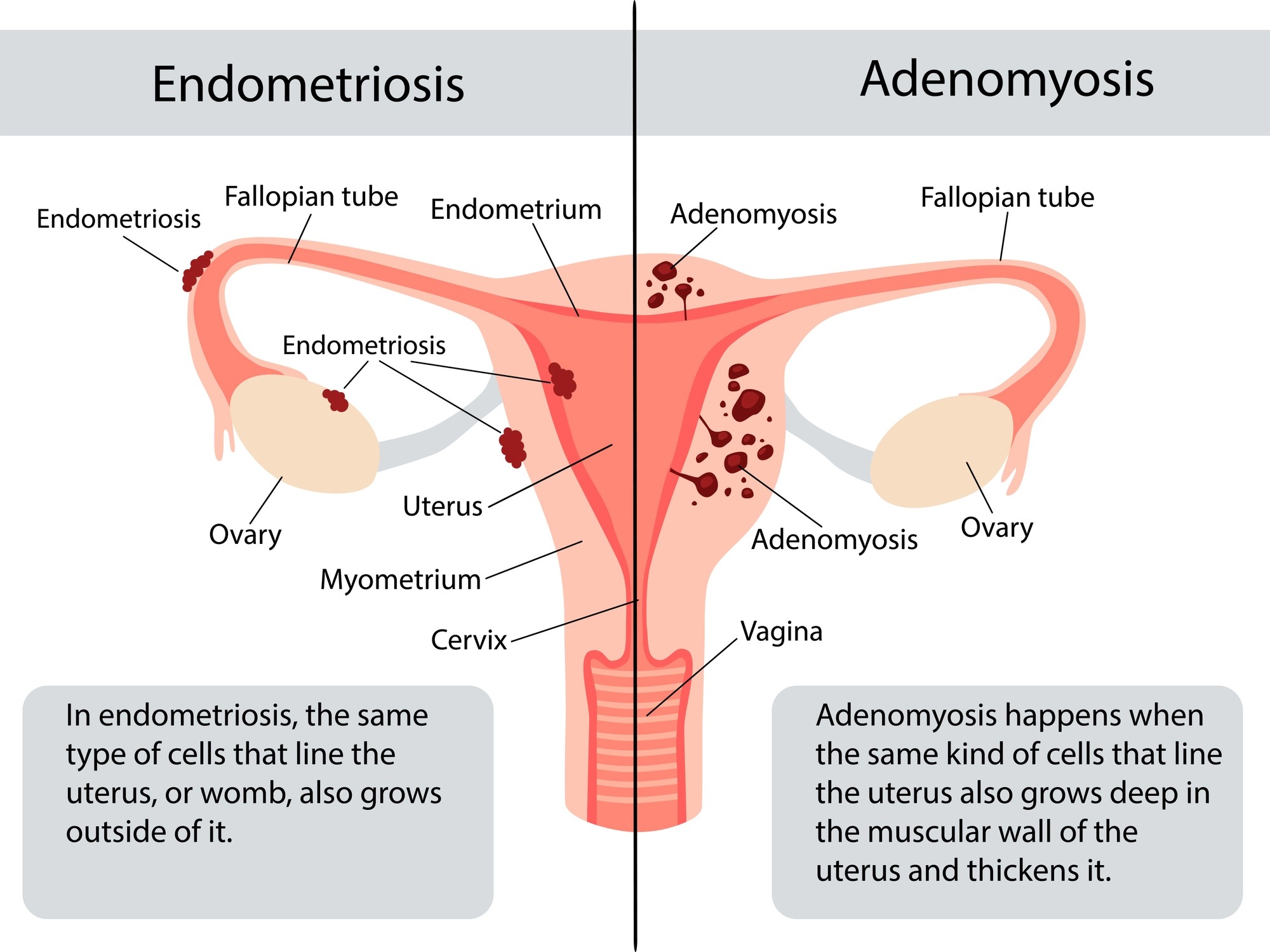
Have you ever felt like your period just won’t quit? Well, you’re not alone. How does one define “heavy periods”? Well, the most appropriate definition is when excessive blood loss interferes with a woman’s physical, emotional and social well-being. Heavy periods, also known as menorrhagia [meh-ner-AY-jee-uh], can happen for various reasons. It might be due to hormones doing a little dance (also known as irregular ovulation), which is common during puberty and perimenopause or certain medical conditions such as polycystic ovarian syndrome (PCOS) and hypothyroidism (underactive thyroid gland). Another cause are non-cancerous growths in the uterus called fibroids and polyps. Conditions like endometriosis (tissue similar to the lining of the uterus grows outside the uterus) and adenomyosis (lining of uterus grows into the muscular wall of the uterus) also join the party, causing a flood of blood each month! Of course, there are also other serious causes not to be missed – such as bleeding disorders (when the blood does not clot properly), medications (such as blood thinners or use of copper IUDs) and endometrial cancer. Any bleeding AFTER menopause (12 months since the last period) is abnormal and requires a visit to your GP, ASAP!
How Common Are Heavy Periods?
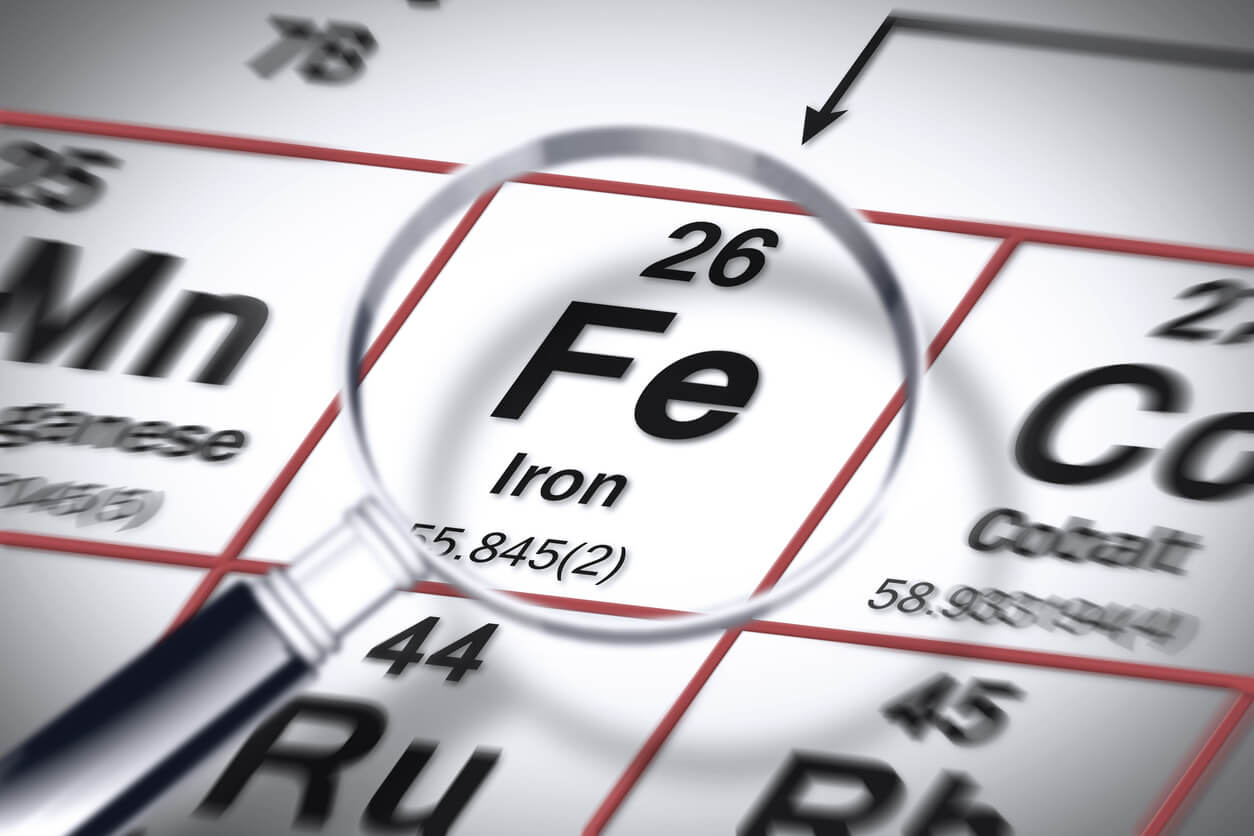
You might be surprised to learn that about one in four women experience heavy periods at some point during their reproductive years1. Despite the prevalence of this issue, many women hesitate to seek help, often due to feelings of embarrassment or the misconception that heavy periods are simply “normal”. In addition, the availability of new feminine hygiene products may give the impression that these symptoms are easily manageable, as these products are designed to accommodate higher volumes of blood. Heavy periods aren’t just about bleeding more—they can make you feel drained, both physically and emotionally (usually from iron depletion and/or anaemia).
Understanding Painful Periods:
Cramps are common during periods, but for some women, the pain is so severe that it prevents them from carrying out their normal daily activities. Pain may be felt as cramping, heaviness or a constant dull ache. This is usually felt in the lower abdomen but can also spread towards the upper abdomen, back and thighs. Some women also experience symptoms of nausea, loose bowel motions and/or dizziness. This painful ordeal is also known as dysmenorrhea [dis-men-uh-ree-uh], and can be caused by excessive contraction of the uterine muscle (primary dysmenorrhea) or due to an underlying condition like endometriosis, adenomysosis or fibroids (secondary dysmenorrhea). Pain in primary dysmenorrhoea usually comes just before or during a period, and usually settles after the first few days of a period. With secondary dysmenorrhoea, the pain can start 1-2 weeks before the period and tends to last longer and/or gets worse over time.
What Can You Do About It?
So, what can you do when faced with heavy periods? The first step is to talk to your GP. We can help figure out what’s causing your symptoms and work with you to find the best treatment options. Initial tests can include a physical examination (and updating your cervical screening test if it is due), blood tests to check iron and red blood cell/haemoglobin levels, thyroid disease and/or bleeding disorders and a pelvic ultrasound to visualise the uterus and ovaries. Fortunately, there are a few treatment options available depending on your age, health and medical history:
- Medication: This can help to reduce bleeding and pain. Medication can come in the form of tablets (hormonal vs. non-hormonal) or an intrauterine device (IUD), which is placed inside the uterus and slowly releases the medication.
- Non-hormonal medication
- Over-the-counter pain relievers like ibuprofen or naproxen can help ease those cramps and make your period more bearable.
- Tranexamic acid is another effective tablet to reduce heavy bleeding by helping blood to clot effectively.
- Hormonal medication
- I.e. the combined oral contraceptive pill (COCP) or Progesterone only pill (POP). These medications act by mimicking the natural hormones in your body – oestrogen and/or progesterone. By doing so, it can be used to skip your period so you experience less bleeding and pain.
- Progesterone intrauterine device (IUD). This is the most effective treatment for heavy and/or painful periods and acts by releasing progesterone locally in the uterus.
- Non-hormonal medication
- Surgery: In severe cases or when medication does not work, surgery such as fibroid removal, endometrial ablation (surgical removal or destruction of the lining of the uterus) or a hysterectomy (removal of the uterus) might be considered.
Together, your GP can help to decide on the most appropriate treatment and if there is a need to collaborate with other specialists, such as a Gynaecologist.
Dealing with heavy or painful periods isn’t easy, but you don’t have to suffer in silence. By understanding the causes and exploring treatment options with your GP, you can take control of your menstrual health and get back to feeling like yourself again. There is hope for a lighter, less painful period ahead!
References:
- Royal College of Obstetricians and Gynaecologists. National heavy menstrual bleeding audit. London: RCOG, 2014.